This article was originally posted on USA Today and Mediaplanet’s “Future of Fertility” highlight.
Infertility affects 15 percent of couples, an estimated 48.5 million couples worldwide. Often couples turn to in vitro fertilization (IVF) to get pregnant.
In the United States, over 81,000 babies were born via IVF in 2018. Over a million babies were born between 1987 to 2015 in the United States as a result of IVF.
Now, innovative genetic testing technology using artificial intelligence (AI), big data, and machine learning is helping advance reproductive medicine.
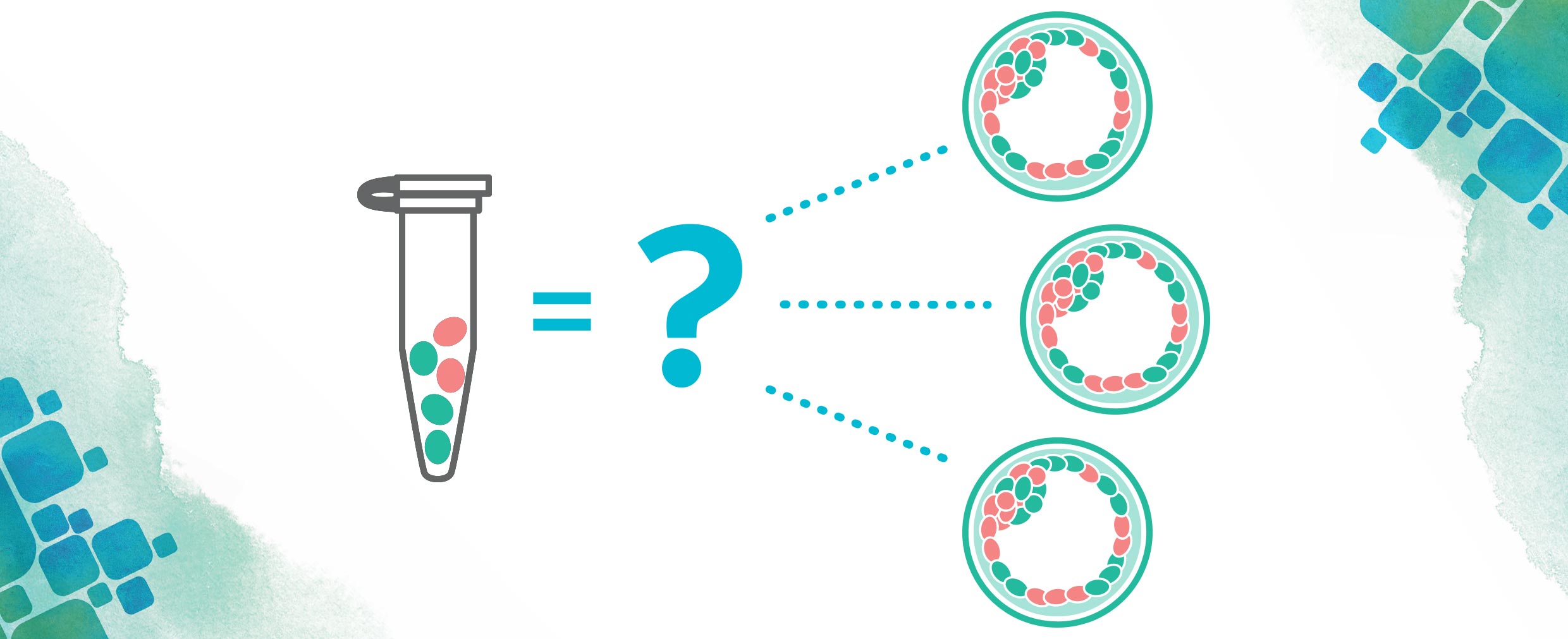
CooperSurgical, a global leader in delivering innovative assisted reproductive technology and genomic solutions, has developed the CooperGenomicsSM PGTaiSM 2.0 technology to screen embryos for IVF. This platform provides advanced accuracy in PGT-A analysis, the preimplantation genetic test that identifies embryos that are chromosomally normal and suitable for transfer, and those that have an abnormal number of chromosomes and may not be suitable for transfer.
Innovative Approach
The ground-breaking PGTai 2.0 technology used the data of more than 1,000 embryos that resulted in a live birth or an ongoing pregnancy as a reference in its development to identify chromosomally normal embryos. In the past, fertility experts relied on human analysts to subjectively screen the embryos. Now the AI can use all those data points and compare the information objectively and efficiently.
“Artificial intelligence helps us to better predict which embryo is more likely to result in a successful pregnancy,” says Tony Gordon, Ph.D., a molecular cytogeneticist and CooperSurgical’s vice president of business development. “With AI, we’re able to look at more data than a human can and look at the embryos in more detail than we were before.”
Screening IVF embryos for chromosome abnormalities before transfer may increase the likelihood of achieving a successful pregnancy, including increasing implantation rates, reducing miscarriage rates, increasing live birth rates, and enabling single embryo transfers.
“The number of abnormal embryos grows with advanced maternal age,” says Dr. Gordon. “But if you can find those embryos, with the right numbers of chromosomes, then a woman in her early 40s will have pretty much the same chance of success as a woman in their early 30s.”
Recent NYU Study
Study results from NYU Langone Fertility Center (NYULFC), part of The Prelude Network, showed increased ongoing pregnancy and live birth rates associated with the use of CooperSurgical’s PGTai 2.0 technology.
“With this study, we saw that these positive outcomes were achieved in one additional embryo out of every 12 transferred,” says Dr. Gordon.
Further results of the study, which included data from 700 patients from NYULFC, suggest that the increase in ongoing pregnancy and live births may be linked to reductions of adverse outcomes, such as miscarriages.
Better Outcomes
“Our whole goal here is to help patients be more successful in their quest for parenthood,” says Jenna Miller, clinical science liaison and genetic counselor at CooperSurgical.
“From a patient’s perspective, IVF is such an emotional roller coaster,” she says. “You go through the process of IVF, which can be an odyssey. And then you get a certain number of eggs, only a certain number of them will fertilize, only a certain number of them make it to point of having genetic testing. And then, only a few of the ones that you test are actually chromosomally normal and capable of making a baby.”
This new technology means that, in addition to improving chances for pregnancy, patients and providers can choose quality over quantity, since the process tells them which embryos are the most viable. That reduces the need to transfer multiple embryos, potentially resulting in a pregnancy with multiple babies, which can be risky for babies and the mother.
“If you are starting the IVF process, you may want to talk to your healthcare team to learn more about the way that they select your embryos and the screening technology that they use,” added Miller.
Author: Kristen Castillo, [email protected]
View original article in the “Future of Fertility” highlight.