In vitro fertilization (IVF) is a popular topic these days, especially given the number of celebrities who have used this method of assisted reproduction. IVF, as you might already know, helps some couples struggling with infertility build their family. However, with the advent of PGT-M, or preimplantation genetic testing for monogenic or single-gene defects, many couples without known fertility issues are turning to IVF to avoid having a child with a genetic disorder.
So, what is this technology used for? PGT-M, (formerly known as preimplantation genetic diagnosis or PGD) evaluates embryos for a specific inherited genetic disorder; this may be a genetic disorder that one of the prospective parents is affected with, or it may be a genetic disorder that one or both parents carries but exhibits no symptoms of. Whatever the case, PGT-M significantly increases the chance that families will have a child unaffected by the genetic disorder in question.
While there is a lot of information about IVF readily available, information about PGT-M may not be as easily accessible to those looking to prevent passing on their specific genetic disorder. If you are considering pursuing PGT-M, here are a couple of things you should know:
1. It (usually) takes a village:
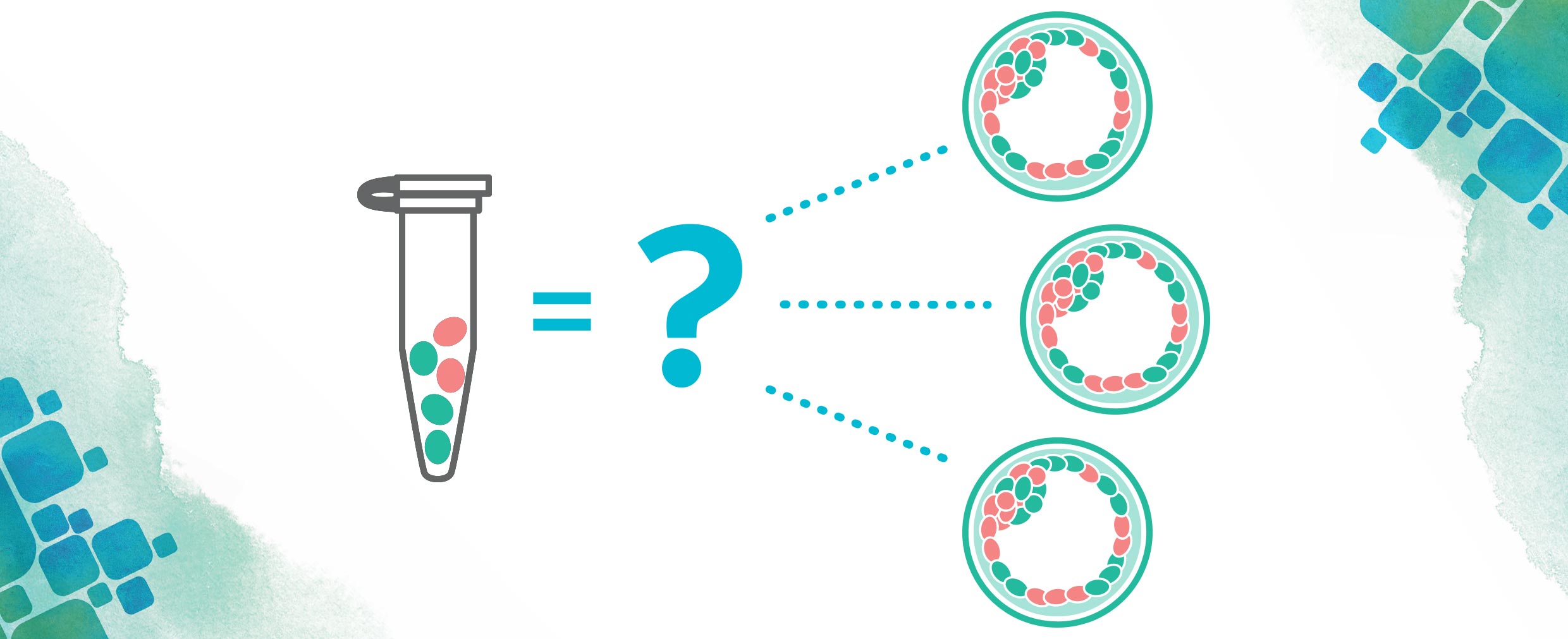
A surprise to most, PGT-M is not done by direct analysis of the disease-causing genetic variant only. There are technical issues that may arise when this type of testing is done on a small DNA sample (and embryo DNA samples are small). While testing for the family-specific variant is often part of testing, a method called linkage analysis is the basis of all PGT-M tests.
Linkage analysis evaluates genetic markers associated with the gene(s) being tested. Because we have two copies of most of our genes, to determine which markers are traveling with each gene, your DNA must be compared to another family member. Each case is unique, but in most cases, the family members who are most informative for linkage analysis are parents or children of the couple. If you do not have family members available to participate in this process, or if you are the only person in your family known to have a genetic disorder, don’t worry; there are other approaches available in most circumstances.
2. In some cases, you can test for disorders for which your own status is uncertain:
In most cases, those pursuing PGT-M know they are carriers of or are affected with a genetic disorder. However, there are circumstances in which embryos may be tested for a genetic disorder that has been identified in the family, but the prospective parent does not know if they are affected. One of the most common disorders this is requested for is Huntington’s disease (HD). Many individuals who are at risk for this genetic disorder choose not to find out if they are affected prior to developing symptoms, but still wish to ensure they do not have an affected child.
For these individuals, PGT-M may be completed using an exclusion approach. In this scenario, embryos are evaluated to determine if the gene(s) in question has been inherited from the affected grandparent or the unaffected grandparent. This identifies embryos at-risk for the genetic disorder in question without revealing the genetic status of the prospective parent. Importantly, because the status of the at-risk parent is not known, embryos identified as at-risk may be unaffected. If an individual completes testing for themselves later, the results of embryo testing may be updated to identify embryos as affected or unaffected.
3. It takes some time:
PGT-M tests are unique; they are designed on an individual-family basis. Even when testing is being completed for a common genetic disorder, such as cystic fibrosis or sickle cell anemia, a large amount of work takes place in the laboratory. On average, it takes at least one month for a test to be ready for use.
4. It might take more than one cycle of IVF to identify an unaffected embryo:
This is probably the hardest thing for couples pursuing PGT-M to hear, but it is one of the most important. Sometimes, during an IVF cycle, the genetic odds do not play out in your favor. While we expect that some embryos will be identified as unaffected by the known genetic disorder, it is possible that testing will indicate that all embryos are affected. This occurs randomly; there is nothing you can do to influence the results. When this occurs, couples must decide if they want to complete another IVF cycle to attempt to get an unaffected embryo.
5. Sometimes it is not possible:
There is a misconception that PGT-M can be used for anything. This is just not true.
Current technologies have limitations and there are some genetic variants for which testing cannot be done. It is always best to consult with the laboratory to determine the feasibility of testing prior to beginning an IVF cycle.
6. It does not test for everything:
PGT-M tests for a specific genetic disorder(s) that your embryos are known to be at risk for. However, it cannot, and does not, test for other disorders that may affect any embryo/child, including birth defects, intellectual disability, and autism. There is no test that may be performed either on an embryo or during pregnancy, that will rule out all potential concerns.
All pregnancies have a 2-4% risk of being affected with a birth defect or genetic disorder. PGT-M may decrease this risk, but it does not eliminate it. Importantly, reproductive technology is always evolving. While we may not have an answer or test for something today, that doesn’t mean it will always remain that way. We encourage patients to stay informed of the latest developments in reproductive technology and to learn how they can help you to plan your future family.
PGT-M may sound like a complicated process and, well, it is. But don’t let it overwhelm you. If you are considering PGT-M, speak with your physician. He/she can help you initiate the process and put you in touch with someone (usually a genetic counselor) who can guide you each step of the way. We share your goal: helping you achieve your healthy family. Knowing your options, knowing what is right for you and your partner, and what will make you both feel empowered along your path to parenthood is something we support! Don’t be afraid to ask questions, do your research, and advocate for yourself. Your future family will thank you!
About the Author: Sheila Johal
 Sheila Johal is a Manager of Laboratory Genetic Counseling at CooperSurgical; she counsels patients seeking preimplantation genetic testing. She came to CooperSurgical after nine and one-half years at MetroHealth Medical Center in Cleveland, Ohio, where she provided prenatal, general, and cardiovascular genetic counseling. Sheila graduated with a master’s degree in Medical and Molecular Genetics with a focus in Genetic Counseling from Indiana University – Purdue University Indianapolis in 2006.
Sheila Johal is a Manager of Laboratory Genetic Counseling at CooperSurgical; she counsels patients seeking preimplantation genetic testing. She came to CooperSurgical after nine and one-half years at MetroHealth Medical Center in Cleveland, Ohio, where she provided prenatal, general, and cardiovascular genetic counseling. Sheila graduated with a master’s degree in Medical and Molecular Genetics with a focus in Genetic Counseling from Indiana University – Purdue University Indianapolis in 2006.
Prior to attending graduate school, she also received a Bachelor of Science in Biology and a Bachelor of Arts in Psychology from Kent State University. She has a specific interest in disorders of hemoglobin, CFTR-related infertility, and is passionate about educating genetic counseling students. She currently serves as co-chair of the OAGC Web Design Subcommittee. When she is not working, Sheila enjoys being with her husband and children, listening to baseball on the radio, baking, and reading.